Manage Care
Care-Based Incentive (CBI) Summary
The Central California Alliance for Health CBI program is comprised of a set of measures to encourage preventive health services and connect Medi-Cal members with their primary care providers (PCPs).
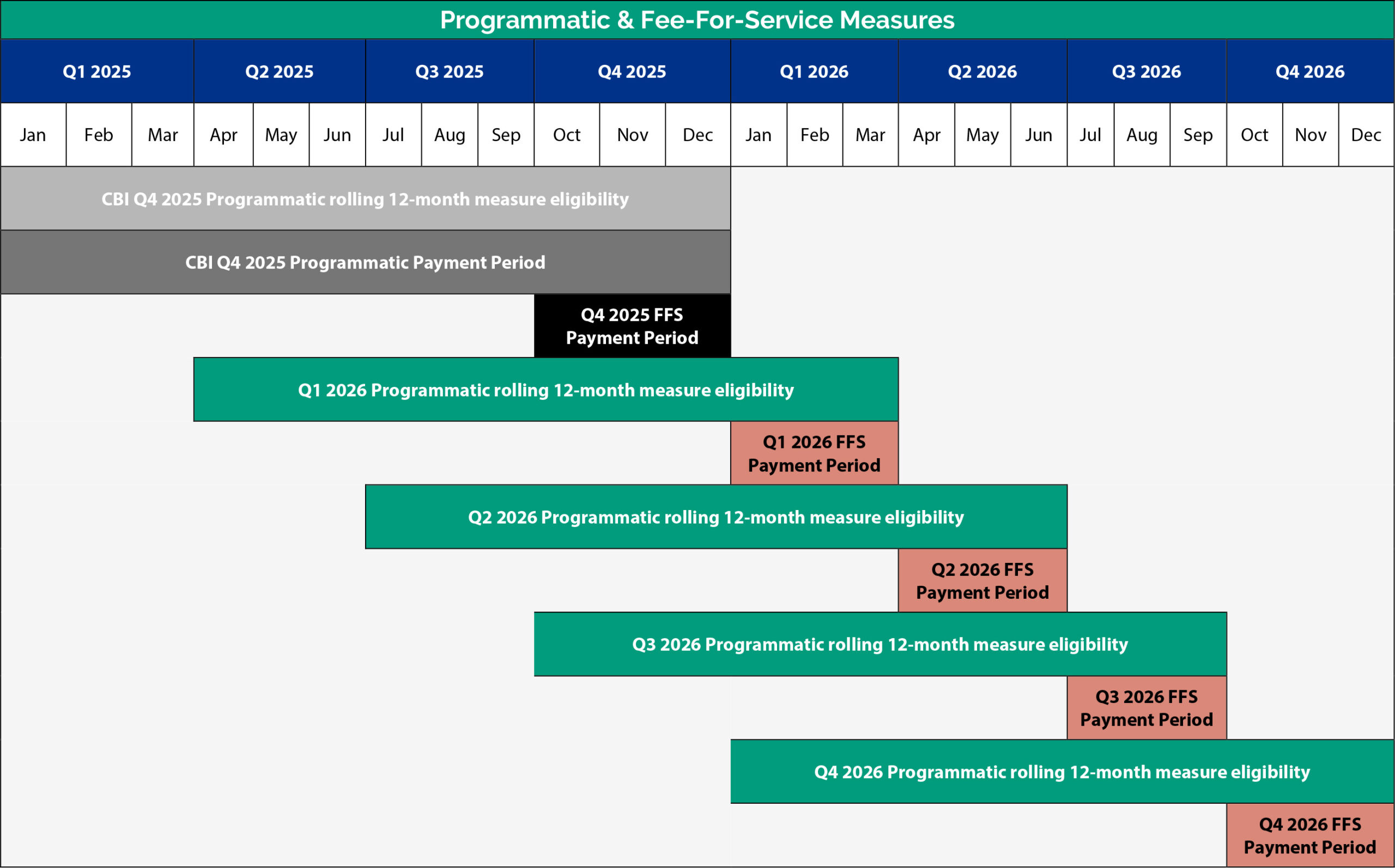
The CBI program consists of provider incentives that are paid to qualifying contracted provider sites, including family practice, pediatrics and internal medicine. Provider incentives are broken into:
- Programmatic measures which are paid annually based on the rate of performance in each measure.
- Fee-for-service (FFS) measures which are paid quarterly when a specific service is performed or a measure is achieved.
This incentive summary provides an overview of the CBI program. For more information about provider incentive payments, refer to the CBI Programmatic Measure Benchmarks and the Alliance Provider Manual.
For additional information on the CBI Program, refer to the program year 2024 and 2025 CBI Technical Specifications. For general questions, contact your Provider Relations Representative or call Provider Relations at 800-700-3874, ext. 5504.
New programmatic measures
The Controlling High Blood Pressure measure moved from exploratory to programmatic and measures members 18-85 years of age who had a diagnosis of hypertension (HTN) and whose blood pressure (BP) was adequately controlled (<140/90 mm Hg) during the measurement year.
The BP reading must occur on or after the date of the second HTN diagnosis.
Measure changes
- The Application of Dental Fluoride Varnish measure now requires at least two topical fluoride applications by the end of the CBI program year and co-located dental practices at Federally Qualified Health Centers (FQHCs) can now submit dental data via the Data Submission Tool.
- The Breast Cancer Screening measure now measures members 40-74 years of age who were recommended for routine breast cancer screening and had a mammogram to screen for breast cancer. The measure also includes gender-affirming codes that can be submitted via the Data Submission Tool.
- The Child and Adolescent Well-Care Visits, Well-Child Visits in the First 15 Months, and Well-Child Visits for Age 15 Months-30 Months of Life measures removed telehealth visits from each of the measure numerators.
- The Immunizations: Adolescents measure now includes the pentavalent meningococcal vaccine for numerator compliance and the age for MCV now begins at 10 years of age.
- The Social Determinants of Health (SDOH) ICD-10 Z Code Submission
fee-for-service measure now accepts all DHCS SDOH ICD-10 Z Codes (All Plan Letter 21-009) and providers now qualify for a $100 payment per member, per provider federal tax ID, per ICD-10 diagnosis code, with a limit of $7,500 per tax ID within the CBI program year.
Coding changes
- The Cervical Cancer Screening measure now includes self-collected HPV testing (87626) and removes in-office pap collection code Q0091. LOINC codes for sex assigned at birth (LOINC code 76689-9) are added, which can exclude members from the measure if the sex assigned at birth (LOINC code 76689-9) is submitted with male (LOINC code LA2-8).
- The Chlamydia Screening measure (previously Chlamydia Screening in Women) accepts LOINC codes for sex assigned at birth, which can exclude members from the measure if the sex assigned at birth (LOINC code 76689-9) is submitted with male (LOINC code LA2-8) or include members if sex assigned at birth (LOINC code 76689-9) is submitted with female (LA-3).
- The Breast Cancer Screening measure added LOINC codes for sex assigned at birth (LOINC code 76689-9), which can include members if the sex assigned at birth (LOINC code 76689-9) is submitted with female (LOINC code LA3-6).
New Programmatic Measures
The following measures were moved from exploratory to programmatic measures:
- Chlamydia Screening in Women.
- Colorectal Cancer Screening.
- Well-Child Visits for Age 15 Months–30 Months of Life.
Measure Changes
Diabetic HbA1c Poor Control >9% changed to Diabetic Poor Control >9%. The measure was modified to review the most recent glycemic status received through hemoglobin A1c [HbA1c] or glucose management indicator [GMI] testing.
Post-Discharge Care
This measure was updated to:
- Accept follow-up care by specialists.
- Exclude members that were admitted to a Skilled Nursing Facility (SNF) on the same day of discharge.
Preventable Emergency Visits
This measure was updated to remove urgent care visits.
Point Allocation Changes
Total allowable points for Quality of Care measures changed from 38 points to 53 points.
Retired Measures
- Health Equity: Child and Adolescent Well-Care Visit.
- Performance Improvement Measure.
| Care Coordination Measures - Access Measures | ||||
|---|---|---|---|---|
| Measure | Summary Definition | Member Eligibility | Resources | Points Possible: 21.5 |
| Adverse Childhood Experiences (ACEs) Screening in Children and Adolescents | The percentage of members one to 20 years of age who are screened for Adverse Childhood Experiences (ACEs) annually using a standardized screening tool. | ≥5 Eligible Linked Members |
Adverse Childhood Experiences (ACEs) in Children and Adolescents Tip Sheet ACE Screening HCPCS codes: |
3 |
| Application of Dental Fluoride Varnish** | The percentage of members six months to five years of age (up to before their sixth birthday) who received at least two topical fluoride applications by staff at the PCP office and/or co-located dental practices at Federally Qualified Health Centers (FQHCs) during the measurement year. | ≥5 Eligible Linked Members |
Application of Dental Fluoride Varnish Tip Sheet Fluoride Application codes: |
2 |
| Developmental Screening in the First Three Years | The percentage of members one to three years of age screened for risk of developmental, behavioral and social delays using a standardized screening tool in the 12 months preceding, or on their first, second or third birthday. |
≥5 Eligible Linked Members |
Developmental Screening in the First Three Years Tip Sheet Developmental Screening CPT code: 96110 |
2 |
| Initial Health Appointment | New members who receive a comprehensive initial health appointment (IHA) within 120 days of enrollment with the Alliance. | ≥5 eligible linked members continuously enrolled within 120 days of enrollment (four months) |
DHCS MMCD Policy Letter 22-030 For a full list of codes, see the Initial Health Appointment Tip Sheet. |
4 |
| Post-Discharge Care | Members who receive a post-discharge visit within 14 days of discharge from a hospital inpatient stay by a linked primary care provider (PCP) or specialist. This measure pertains to acute hospital discharges only. Emergency room visits do not qualify. | ≥5 Eligible Linked Members |
Post-Discharge CPT Codes: 99202-99215, 99241-99245, 99341- 99350, 99381-99385, 99391-99395, 99429 |
10.5 |
| Care Coordination Measures – Hospital and Outpatient Measures | ||||
| Measure | Summary Definition | Member Eligibility | Resources | Points Possible: 25.5 |
| Ambulatory Care Sensitive Admissions |
The rate of ambulatory care sensitive admissions per 1,000 eligible members per year. The list of conditions is based on plan-identified AHRQ specifications. Note: This is an inverse measure; a lower rate of admissions qualifies for more CBI points. |
≥100 Eligible Linked Members |
Ambulatory Care Sensitive Admissions Tip Sheet For a full list of codes see the CBI Technical Specifications |
7 |
| Plan All-Cause Readmission |
The number of members 18 years of age and older with acute inpatient and observation stays during the measurement year that was followed by an unplanned acute readmission for any diagnosis within 30 days. Note: This is an inverse measure; a lower rate of readmissions qualifies for more CBI points. |
≥100 Eligible Linked Members |
Plan All-Cause Readmission Tip Sheet For a full list of codes see the CBI Technical Specifications |
10.5 |
| Preventable Emergency Visits |
The rate of preventable emergency department (ED) visits per 1,000 eligible members per year. Note: This is an inverse measure; a lower rate of preventable ED visits qualifies for more CBI points. |
≥100 Eligible Linked Members | 8 | |
| Quality of Care Measures | ||||
| Measure | Summary Definition | Member Eligibility | Resources | Points Possible: 53 |
| Breast Cancer Screening** | The percentage of members 40-74 years of age who were recommended for routine breast cancer screening and had a mammogram to screen for breast cancer on or between October 1 two years prior to the measurement period and the end of the measurement period. | ≥30 Eligible Linked Members |
Breast Cancer Screening Tip Sheet Breast Cancer Screening CPT Codes: For a full list of codes see the CBI Technical Specifications |
Varies |
| Cervical Cancer Screening |
The percentage of members 21-64
Note: When testing for hrHPV or cotesting for cervical cancer, members must be 30-64 years of age or older on the date of the test. |
≥30 Eligible Linked Members |
Cervical Cancer Screening Tip Sheet Cervical Cytology CPT codes: 88141-88143, 88147-88150, 88152-88153, 88164-88167, 88174-88175 hrHPV CPT codes: 87624-87626 To exclude members from the measure: Sex assigned at birth (DST submission only): Sex Assigned at Birth (LOINC code 76689-9) of Male (LOINC code LA2-8) For a full list of codes see the CBI Technical Specifications |
Varies |
| Child and Adolescent Well-Care Visits (Three to 21 years)** | The percentage of members three to 21 years of age who had at least one comprehensive well-care visit with a PCP or an OB/GYN practitioner during the measurement year. |
≥30 Eligible Linked Members |
Child and Adolescent Well-Care Visits Tip Sheet Well-Visit codes: |
Varies |
| Chlamydia Screening** | The percentage of members 16-24 years of age who were recommended for routine chlamydia screening, identified as sexually active and had at least one test for chlamydia during the measurement year. | ≥30 Eligible Linked Members |
Chlamydia Screening CPT codes: Sex assigned at birth LOINC codes (DST submission only): Sex assigned at birth (76689-9) of male (LA2-8) |
Varies |
| Colorectal Cancer Screening* |
The percentage of members 45-75 years of age who had appropriate screening for colorectal cancer. For members 46-75 years of age, use any of the following criteria:
|
≥30 Eligible Linked Members |
Colorectal Cancer Screening Tip Sheet Fecal occult blood test CPT codes: 82270, 82274 Flexible sigmoidoscopy CPT codes: 45330-45335, 45337, 45338, 45340-45342, 45346, 45347, 45349, 45350 Colonoscopy CPT codes: 44388-44394, 44401-44408, 45378-45382, 45384-45386, 45388-45393, 45398 CT colonography CPT codes: 74261-74263 Stool DNA (sDNA) with FIT CPT code: 81528 |
Varies |
| Controlling High Blood Pressure* |
The percentage of members 18-85 years of age who had a diagnosis of hypertension (HTN) and whose blood pressure (BP) was adequately controlled (<140/90 mm Hg) during the measurement year. BP reading must occur on or after the date of the second HTN diagnosis. |
≥30 Eligible Linked Members |
Controlling High Blood Pressure Tip Sheet Controlling High Blood Pressure Codes: |
|
| Depression Screening for Adolescents and Adults | The percentage of members 12 years of age and older who are screened for clinical depression using an age-appropriate standardized tool, performed between January 1 and December 1 of the measurement period. | ≥30 Eligible Linked Members |
Depression Screening for Adolescents and Adults Tip Sheet Depression Screening Tool LOINC codes (DST submission only; must include result): Pediatric: 89205-9, 89204-2 Adult: 89209-1, 89205-5, 90853-3, 48545-8, 48544-1, 90221-3, 71777-7 Pediatric & Adult: 89208-3, 55758-7, 44261-6, 71965-8, 99046-5 |
Varies |
| Diabetic Poor Control >9% |
The percentage of members 18-75 years of age with diabetes (type 1 and type 2) whose most recent glycemic assessment (hemoglobin A1c [HbA1c] or glucose management indicator [GMI]) was >9% in the measurement year. The measure goal is for members to be non-compliant by having an HbA1c or GMI of equal to or less than 9% and being in good control (a lower rate indicates better performance). Members with no lab or no lab value submitted, a claim without an HbA1c value or an HbA1c value >9% is considered compliant for this measure. |
≥30 Eligible Linked Members |
Diabetic HbA1c Poor Control >9% Tip Sheet CPT codes: 83036, 83037 (Non Medi-Cal benefit code) LOINC codes: 17855-8, 17856-6, 4548-4, 4549-2, 96595-4, 97506-0 CPT II result codes (Point of Service Labs): 3044F, 3046F, 3051F, 3052F |
Varies |
| Immunizations: Adolescents** | The percentage of adolescents 13 years of age who had one dose of meningococcal vaccine, one dose of tetanus, diphtheria toxoids and acellular pertussis (Tdap) vaccine and completed the human papillomavirus (HPV) vaccine series by their 13th birthday. | ≥30 eligible linked members |
Immunizations: Adolescents Tip Sheet Immunization CPT Codes: |
Varies |
| Immunizations: Children (Combo 10) |
The percentage of children who received all of the following 10 vaccines by their second birthday:
|
≥30 Eligible Linked Members |
Immunizations: Children (Combo 10) Tip Sheet For a full list of codes see the CBI Technical Specifications |
Varies |
| Lead Screening in Children | The percentage of children two years of age who had one or more capillary or venous lead blood test for lead poisoning by their second birthday | ≥30 Eligible Linked Members |
Lead Screening in Children Tip Sheet Lead Screening CPT code: 83655 For a full list of codes see the CBI Tech Specs. |
Varies |
| Well-Child Visits in the First 15 Months** | The percentage of members 15 months of age who had six or more well-child visits with a PCP during the first 15 months of life. | ≥30 Eligible Linked Members |
Well-Child Visits in the First 15 Months Tip Sheet Well-Child Visit codes: |
Varies |
| Well-Child Visits for Age 15 Months-30 Months of Life | The percentage of members 30 months of age who had two or more well-child visits with a PCP between the child’s 15-month birthday plus one day and the 30-month birthday. | ≥30 Eligible Linked Members |
Well-Child Visits for Age 15 Months-30 Months of Life Tip Sheet Well-Child Visit codes: |
Varies |
* New measure for 2026 ** Measure change for 2026
| Practice Management Measures | ||
|---|---|---|
| Measure | Summary Definition | Resources |
| Adverse Childhood Experiences (ACEs) Training and Attestation | Plan pays providers, which includes mid-level providers, for completing the DHCS ACEs training and attestation. The plan pays $200 to each group that the provider practices under. |
$200 one-time payment after receipt of state notification of training and attestation completion. Payments do not reoccur yearly or quarterly. |
| Behavioral Health Integration | Plan pays a $1,000 one-time payment to providers for achievement of NCQA Distinction in Behavioral Health Integration. Payments are made a single time after distinction is received by the Alliance. |
$1,000 one-time payment for achievement of NCQA Distinction in Behavioral Health Integration. Payments do not reoccur yearly or quarterly. |
| Cognitive Health Assessment Training and Attestation | Plan pays providers, which includes mid-level providers, for completing the DHCS cognitive health assessment training and attestation. The plan pays each group $200 that the provider practices under. |
$200 one-time payment after receipt of state notification of training and attestation completion. Payments do not reoccur yearly or quarterly. |
| Diagnostic Accuracy and Completeness Training | Plan pays providers for completing the CMS Diagnostic Accuracy and Completeness Training. |
$200 one-time payment after receipt of certification notification of training completion. Payments do not reoccur yearly or quarterly. |
| Quality Performance Improvement Projects | Plan pays providers $1,000 for each office that completes an Alliance-offered Quality Performance Improvement Project. Only offices with metrics below the minimum performance level, measured at the 50th percentile for the 2025-year programmatic payment are eligible for payment for completion of Quality Performance Improvement Projects. |
$1,000 one-time payment after notification of project completion. Payments do not reoccur yearly or quarterly. |
| Patient-Centered Medical Home (PCMH) Recognition | Plan pays a one-time payment of $2,500 to providers for achievement of NCQA recognition or The Joint Commission (TJC) certification. A copy of the recognition/certification must be received by the Alliance. |
$2,500 one-time payment. Payments do not occur yearly or quarterly. For providers submitting their initial application for NCQA PCMH Recognition, use Alliance discount code CCAAHA to save 20% on your initial application fee. |
| Social Determinants of Health (SDOH) ICD-10 Z Code Submission** | Plan pays PCPs who submit claims using the DHCS SDOH ICD-10 Z Codes (All Plan Letter 21-009). Providers qualify for a $100 payment per member, per provider federal tax ID (EIN), per ICD-10 diagnosis code for claim submissions with a DHCS SDOH Z diagnosis code, not to exceed $7,500 per tax ID within the CBI term. |
$100 per member, per provider federal tax ID (EIN), per ICD-10 diagnosis code for claim submissions with a DHCS SDOH Z diagnosis code, not to exceed $7,500 per tax ID within the CBI term. |
* New measure for 2026 ** Measure change for 2026
Note: The IHA incentive has a 15-month measurement period to accommodate 120 days post-enrollment date. See CBI Technical Specifications for additional information.
Questions?
Contact your Provider Relations Representative or call Provider Services at 800-700-3874, ext. 5504
Contact us | Toll free: 800-700-3874