The Alliance is required to submit encounter data to the Department of Health Care Services (DHCS). In order to comply with DHCS requirements, all primary and secondary claims for Physician Administered Drugs (PAD) must be billed with a qualifier, National Drug Code (NDC), unit of measure and quantity.
Units of measure include qualifier F2 (International Unit), GR (Gram), ML (Milliliter), and UN (Unit). How do I submit a claim that includes a qualifier, NDC, unit of measure and quantity?
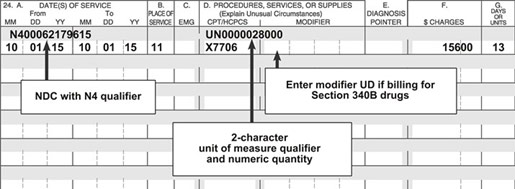
- Hardcopy submission on a CMS-1500 claim form:
- Shaded area of Box 24: enter product ID qualifier (omit space & hyphens) and the 11- digit NDC Directly following the last digit of the NDC, enter the two-character unit of measure qualifier followed by the numeric quantity.
- Example of correct claim billing:
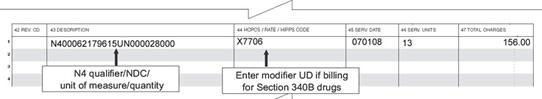
- Hardcopy submission on a UB-04 claim form:
- Field 43: enter product ID qualifier (omit space & hyphens) and the 11-digit NDC Directly following the last digit of the NDC, enter the two-character unit of measure qualifier followed by the numeric quantity (A nine digit number. The nine digits consist of six digits for the whole number, followed by three decimal places.)
- Example of correct claim billing:
- EDI submission for Professional (837p) and Institutional (837i) Claims:
Loop Segment Element Name o 2410 LIN Product or Service ID Qualifier o 2410 LIN Product or Service ID o 2410 CTP Quantity o 2410 CTP Unit or Basis for Measurement Code
Unit of measure and quantity are currently not required for direct submission to the Alliance or DHCS per Medi-Cal guidelines and therefore omitting such data will not result in claim denial. However, in the near future claims lacking unit of measure and quantity will be denied. The denial reason will be 522 – physician administered drug information missing or invalid.
This memo is a courtesy notice to urge providers to make the appropriate billing modifications now before such billing prompts claim denials. Additional noticing of this billing requirement will be sent out to providers following our standard noticing timeframes.
If you have any questions or need more information, please contact the Alliance Claims department at (800) 700-3874, ext. 5503.


