
Manage Care
Preventable Emergency Visits Tip Sheet
Measure Description:
The rate of preventable emergency (ED) and urgent visits per 1,000 members per year. This measure is derived from the Statewide Collaborative Quality Improvement Project: Reducing Avoidable Emergency Room Visits.
Incentives will be paid on an annual basis, following the end of Quarter 4. For additional information refer to the CBI Technical Specifications.
Members are frequently seen at the ED or urgent care for screening services and general examinations. Below is a list of common preventable ED and urgent care diagnoses derived from the Statewide Collaborative Quality Improvement Project: Reducing Avoidable Emergency Room Visits.
- Acute bronchitis, nasopharyngitis, upper respiratory infection, pharyngitis
- Sore mouth or throat (e.g., thrush, tonsillitis), ear infections
- Allergies, sinusitis, conjunctivitis
- Back pain
- Headache
- Skin problems/infections (scabies, miliaria, tinea corporis)
- Urinary tract infection
- Vaginitis
For a full list of preventable diagnoses, see Preventable Emergency Visit Diagnosis Tip Sheet on the website and the 2022 and 2023 CBI Technical Specifications.
Educate All Members To:
- Use the Alliance’s Nurse Advice Line – available to all Alliance members 24 hours a day, 7 days a week, 365 days a year.
- Always call the PCP office for an appointment before going to the ED or urgent care.
Assign Clinic Staff To:
- Monitor the Provider Portal Linked Member ED Visit report as a tool for tracking linked members who were recently seen in the ED, as well as the Linked Member High ED Utilizers for members seen in the ED three or more times within a 90-day period. There may be members who are assigned who have never been seen to whom you can provide additional outreach.
- Contact members seen for preventable ED or urgent care visits and bring them in for follow-up.
- Review day-of-the-week trends and open additional appointment times based on trends.
- Look at your third next available appointment times; if appointments are too far out, patients are more likely to use the ED.
- Orient all new members on your office hours, how to reach you after hours, and what kinds of conditions you will see urgently.
- Route after hours calls for Alliance members to the Alliance’s Nurse Advice Line: 1 (844) 971-8907.
- Identify high utilizers of the ED and bring them in to review their problem list.
- Refer Alliance Members to Care Management Services, including Complex Case Management and Care Coordination, by calling Case Management at (800) 700-3874 ext. 5512.
- Refer Alliance Members to Enhanced Care Management (eCM) and Community Supports using the Enhanced Care Management Provider Referral Form or the Community Supports Provider Referral Form.
- Refer Alliance Members to behavioral health services through Carelon Behavioral Health using the Carelon Behavioral Health Primary Care Provider (PCP) Referral Form.
- Alliance interpreting services are available to network providers:
- Telephonic interpreting services are available to assist in scheduling members.
- Face-to-face interpreters can be requested to be at the appointment with the member.
For information about our Cultural and Linguistic Services Program, please call the Alliance Health Education Line at 800-700-3874, ext. 5580 or email us at [email protected].
- Refer Alliance Members that have transportation challenges to the Alliance’s Transportation Coordinator at 1-800-700-3874 ext. 5577; this service is not covered for non-medical locations or appointments that are not medically necessary.
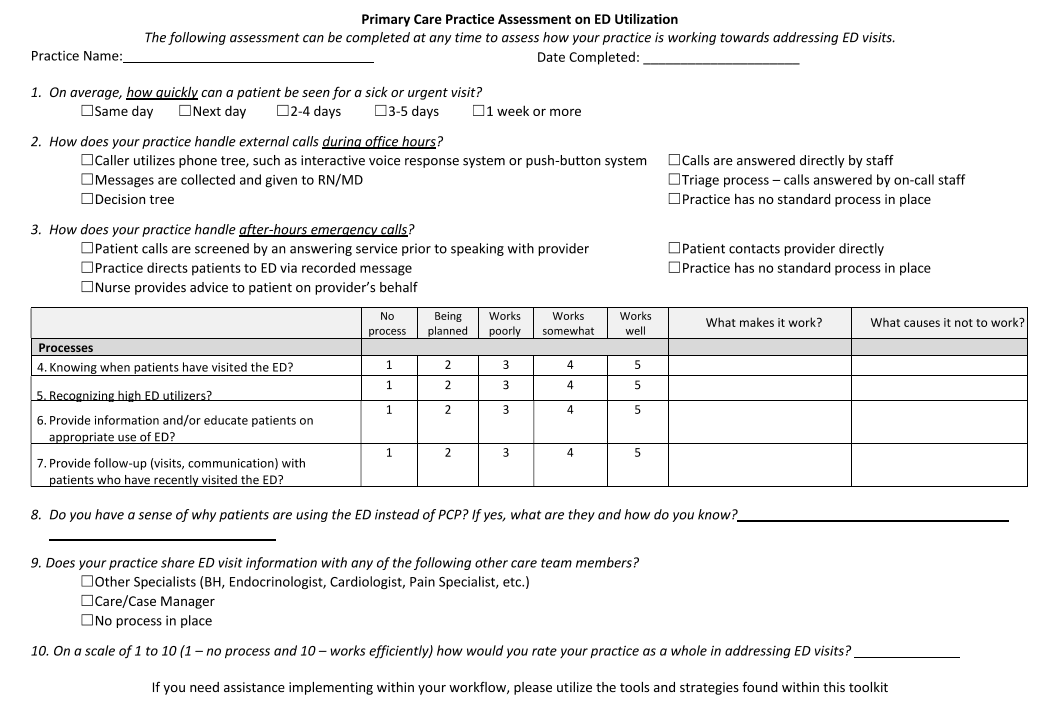
- Impacting Use of the Emergency Department Physician Toolkit and PCP Assessment Tool:
Reference: Harvey, MD, B. Washington Chapter. American Academy of Pediatrics. Retrieved from https://wcaap.org/wp-content/uploads/2021/09/Impacting-Use-of-the-Emergency-Department-final.pdf
Contact us | Toll free: 800-700-3874

